What is Epinephrine?
Epinephrine, also known as adrenaline, is a monoamine that functions as both a stress hormone and excitatory neurotransmitter. A monoamine is an amino group connected to an aromatic ring by a two-carbon chain. Epinephrine is also one of the three neurotransmitters known as a catecholamine – dopamine and norepinephrine being the other two. Epinephrine is a potent agonist of both alpha (α1 and α2) and beta (ß1 and ß2) adrenergic receptors,1 i.e., a stress hormone that powerfully stimulates the sympathetic nervous system.
Most of the epinephrine in the body operates as a hormone secreted by the adrenal glands during acute stress, its stimulatory effects working to prepare an individual to either fight or flee. A comparatively small amount acts as a neurotransmitter, produced in and secreted by neurons of the sympathetic nervous system.
What Does Epinephrine Do to The Body?
The sum of epinephrine’s effects is to rapidly provide the body with the energy and alertness necessary to produce an appropriate response to stressors. It does this by binding to alpha and beta adrenergic receptors throughout the body and changing how the following organs function.
Heart and Blood Vessels
Epinephrine increases the rate and force of cardiac contractions, increasing blood pressure and blood flow. And while blood vessels constrict throughout the body, they dilate in key areas where increased blood flow will be needed, such as in skeletal muscle and the liver.
Muscles
Skeletal muscles receive additional blood flow and resources, enabling one to physically react quickly and forcefully.
Lungs
Smooth muscles in the lungs are relaxed under the action of epinephrine, dilating bronchial tubes (bronchodilation) and increasing oxygen intake.
Liver
Glucose levels in the blood increase both by initiating glycogenolysis, the breakdown of glycogen, and by gluconeogenesis, the production of glucose in the liver. Levels of free fatty acids are also increased. The extra glucose and fatty acids provide fuel for the body.
Eyes
Dilator muscles in the eye constrict, dilating the pupils for improved visual acuity.
Digestion
Blood flow to the gut decreases and the smooth muscles of the stomach and intestines relax, slowing, or even halting digestion.2
Where is Epinephrine Found in the Body?
Most of the body’s epinephrine is produced by chromaffin cells within the adrenal medulla of the adrenal gland. From there, epinephrine acts as a hormone and is secreted directly into the bloodstream.
The comparatively small amount of epinephrine that serves as a neurotransmitter is produced by neurons of the sympathetic nervous system. It has only a small role as a CNS neurotransmitter.
Within the adrenomedullary cells of the adrenal glands, sympathetic neurons, and specific centers of the brain, catecholamine synthesis begins with the uptake of the amino acid tyrosine (Tyr) into the cytoplasm. Through a series of enzymatic reactions, tyrosine is converted into L-Dopa, then dopamine, then norepinephrine, then epinephrine. Tyrosine is produced via hydroxylation of phenylalanine in the liver or it comes from the diet.4
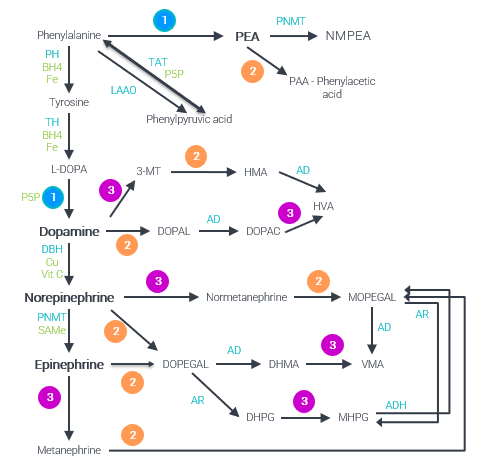 Catecholamine Pathway. Phenylalanine and tyrosine are the precursor amino acids for the catecholamines. In a series of biochemical steps, it is converted to tyrosine, L-DOPA, dopamine, norepinephrine, and then epinephrine. Cofactors work with enzymes to synthesize the neurotransmitters and break them down. These include tetrahydrobiopterin (BH4), iron, copper, vitamin C, vitamin B6, magnesium, and s-adenosylmethionine (SAMe).
Catecholamine Pathway. Phenylalanine and tyrosine are the precursor amino acids for the catecholamines. In a series of biochemical steps, it is converted to tyrosine, L-DOPA, dopamine, norepinephrine, and then epinephrine. Cofactors work with enzymes to synthesize the neurotransmitters and break them down. These include tetrahydrobiopterin (BH4), iron, copper, vitamin C, vitamin B6, magnesium, and s-adenosylmethionine (SAMe).
Enzymes and Cofactors found in Multiple Monoamine Pathways 1) Aromatic L-amino acid decarboxylase (AADC) + Vitamin B6 2) Monoamine oxidase (MAO) + Vitamin B2 3) Catechol-O-Methyltransferase (COMT) + Magnesium + S-adenosylmethionine (SAMe) Neurotransmitters and Metabolites DHPG: 3,4-dihydroxyphenylglycol, DHMA: 3,4-dihydroxymandelic acid, DOPAC: 3,4-dihydroxyphenylacetic acid, DOPAL: 3,4-dihydroxyphenylacetaldehyde, DOPEGAL: 3,4-dihydroxyphenylglycolaldehyde, HMA: 4-hydroxy-3-methoxyphenylacetaldehyde / homovanillin, HVA: homovanillic acid, MHPG: 3-methoxy-4-hydroxyphenylglycol (aka MOPEG), MOPEGAL: 3-methoxy-4-hydroxyphenylglycolaldehyde, NMPEA: N-Methylphenethylamine, VMA: vanillylmandelic acid, 3-MT: 3-methoxytyramine, Enzymes AD: aldehyde dehydrogenase, ADH: alcohol dehydrogenase, AR: aldehyde reductase, DBH: Dopamine Beta-Hydroxylase, LAAO: L-amino-acid oxidase, PH: alanine Hydroxylase, PNMT: phenylethanolamine N-methyltransferase, TAT: Tyrosine aminotransferase, TH: Tyrosine hydroxylase, Cofactors BH4: Tetrahydrobiopterin, Fe: Iron, SAMe: S-adenosylmethionine, Vit: Vitamin
How Do Epinephrine and Hormones Interact?
Epinephrine works with norepinephrine to activate the HPA axis, the body’s stress response system. Epinephrine serves as the initiator, after which norepinephrine takes over the sustained stress response effort. This is epinephrine’s main role, as a hormone of the stress response.
A deficiency in cortisol, a key part of the body’s stress response, decreases epinephrine levels. Cortisol stimulates PNMT, the enzyme that converts norepinephrine to epinephrine.
Epinephrine can stimulate insulin via its beta receptors, but its dominant effect (via alpha receptor activation) is an inhibition of insulin secretion. Thus, EPI contributes to hyperglycemia during stressful situations, both by stimulating glycogenolysis and gluconeogenesis and by an overall inhibiting effect on insulin secretion.
How Does Epinephrine Become Imbalanced?
Stress
The definition of a stressful situation may have changed over the past thousand years, but our body’s response to it has not. Traffic jams, family troubles, polarizing political commentary, unpleasant work – these stressors are just as capable of activating the fight-or-flight response as a buffalo stampede would have 200 years ago.
For the most part, today’s stressors are not life-threatening, but They’re more common than stressors of the past.
Epinephrine’s job is to activate the fight-or-flight response, not sustain it. The HPA axis, a network consisting of the hypothalamus (H), pituitary gland (P), and the adrenal glands (A), sets off a cascade of stress hormones in response to the initial surge of epinephrine.
When the threat eventually passes, cortisol levels will fall, heart rate and blood pressure will return to normal, and other affected organ systems will resume their normal activity. However, frequent surges of epinephrine can damage blood vessels, increase blood pressure, and increase the risk of a heart attack or stroke.
Elevated levels of cortisol can impact blood sugar levels, weight management, immune system activity, digestion, and even erectile function and the menstrual cycle.5,6
Other causes of epinephrine imbalance include:
Maldigestion or malabsorption. Problems digesting and using nutrients from the diet can make it difficult for the body to produce epinephrine. Amino acids, B vitamins, and minerals are required for the body to produce healthy levels of epinephrine.
Hormone imbalances. Epinephrine is a key part of the HPA axis and when other hormones are imbalanced, it can throw off epinephrine levels as well. Cortisol and insulin are known to interact with epinephrine.
Methylation problems. To make epinephrine and dispose of it, the body needs to move around small chemical groups called “methyl groups.” This process doesn’t work optimally in all people and requires B vitamins, S-adenosylmethionine (SAMe) and, for epinephrine production, adequate cortisol.
What are the Warning Signs of an Epinephrine Imbalance?
LOW epinephrine levels have been associated with:
- Anxiousness
- Decreased mood
- Headaches
- Difficulty sleeping
- Poor blood sugar management
- Changes in blood pressure and heart rate
HIGH epinephrine levels can cause:
- Changes in blood pressure
- Changes in heart rate
- Increased sweating
- Cold and/or pale skin (from constriction of blood vessels)
- Shakiness or jitters
- Headaches
Although rare, pheochromocytomas, neuroblastomas, and paragangliomas are tumors that can increase catecholamine secretion and cause high epinephrine levels. They are found in and around the adrenal gland. These types of tumors are diagnosed by biopsy and elevated 24-hour urinary catecholamines.7
What’s the Difference Between Epinephrine and Norepinephrine?
Epinephrine and norepinephrine are catecholamines that operate both as a hormone and as a neurotransmitter for the sympathetic nervous system. The key difference is that epinephrine’s primary function is as a hormone, to activate fight-or-flight. Norepinephrine, particularly as a neurotransmitter, has additional responsibilities in other aspects of our health, such as attention, focus, and sleep regulation. Other differences are listed below.
Molecular Structure
Epinephrine (adrenaline) is actually produced by the methyltransferase enzyme PNMT, adding a single methyl group (CH3) to norepinephrine (noradrenaline), a process known as methylation. That simple -CH3 is all that distinguishes between them at a molecular level.
Production Site
The majority of epinephrine is produced in the adrenal medulla within the adrenal glands, with a small amount being produced by the sympathetic nervous system.
The reverse is true for norepinephrine. The majority is produced in the periphery by sympathetic postganglionic fibers, and in the CNS in the locus coeruleus, with a comparatively small amount being produced by the adrenal medulla.
Release Frequency
Epinephrine is only released into the bloodstream in times of stress, (including hypoglycemic episodes) to trigger the fight-or-flight response. Norepinephrine is released continuously.
Receptor Affinity
Adrenergic receptors are those that bind adrenergic agonists such as norepinephrine and epinephrine. Norepinephrine binds to α1, α2, and ß1 adrenergic receptors. Epinephrine binds to every adrenergic receptor (α1 and α2, ß1 ß2 and ß3),8 and has a greater affinity for ß1 than norepinephrine.
Role in Fight-or-Flight
Epinephrine, as a hormone, acts on most body tissues, increasing heart rate and blood pressure, opening airways in the lungs, breaking down glycogen to raise glucose, dilating the pupils, etc. Norepinephrine’s role mirror’s epinephrine’s role, increasing heart rate, vasoconstricting to raise blood pressure, breaking down fat and increasing glucose. Together they prepare the body to fight or flee.
How Can You Identify an Epinephrine Imbalance?
The neurotransmitter urine test performed by NeuroLab® uses Ultra-high Performance Liquid Chromatography (UHPLC) coupled with Triple Quadruple Mass Spectrometry (QQQ-MS), which offers the highest level of specificity and sensitivity for neurotransmitter testing available on the market.
Whereas standard high-pressure liquid chromatography (HPLC) has a detection limit measured in nanograms (one-billionth of a gram), NeuroLab®’s technology has a limit of detection quantified by picograms, or one-trillionth of a gram.9
With a simple test kit shipped to one’s home, NeuroLab® can offer an accurate snapshot of brain chemistry without the need to draw blood, or even leave home.
How Can You Naturally Support Epinephrine Balance?
Low epinephrine or high epinephrine levels can be corrected through diet and lifestyle. Low levels of epinephrine indicate that a person isn’t getting enough of the building blocks and cofactors needed to manufacture the neurotransmitter. High levels suggest that the fight-or-flight response is activated and stress reduction techniques are needed.
Relaxation Response
Lower epinephrine levels with deep abdominal breathing, focusing on a soothing word such as “peace” or “calm,” visualizing scenes of tranquility, meditation, yoga, tai chi, or any other activity that has a calming effect.
Exercise
Physical activity naturally deepens breathing and helps to relieve muscle tension. Tai Chi and yoga can be doubly effective as they combine movement with deep breathing and mental focus, which can have a profound calming effect.
Social Support
There’s no substitute for the emotional support of friends and family during times of stress and anxiety.
Sleep
The HPA-axis is involved in the stress response and in sleep-wake cycles. Getting enough sleep is critical for healthy function of the HPA axis.
Time Management
Reduce stress by being more organized, prioritizing how you spend your time, and removing superfluous tasks.
Dietary Supplements Can Balance Epinephrine Levels
- Amino acid precursors L-phenylalanine and/or L-tyrosine are the amino acid building blocks for epinephrine and may be helpful to increase low epinephrine levels.*10
- Cofactors such as B vitamins and minerals (iron, magnesium and copper) are required by the body to produce epinephrine and break it down. Improving nutrition and adding supplements to provide cofactors could balance epinephrine.*
- Integrative and functional medicine practitioners often use herbal supplements to modulate the HPA axis, especially when cortisol levels are high. Examples of these treatments include: panax ginseng, phosphatidylserine, rhodiola, and ashwagandha.*11
References
- Feher J. Cells, Synapses, and Neurotransmitters. In: Quantitative Human Physiology. 2nd ed.: Academic Press; 2016:1008.
- Romero LJ, Butler LK. International Journal of Comparative Psychology. 2007;20:89-95.
- Robertson D, ed Primer on the Autonomic Nervous System. Academic Press; 2012.
- Joseph JJ, Golden SH. Ann N Y Acad Sci. 2017;1391(1):20-34.
- Salvio G, Martino M, et al. J Clin Med. 2021;10(12).
- Davison AS, Jones DM, et al. Ann Clin Biochem. 2018;55(1):34-48.
- Farzam K, Kidron A, et al. Adrenergic Drugs. In: Treasure Island, FL: StatPearls Publishing; 2022: https://www.ncbi.nlm.nih.gov/books/NBK534230/. Accessed 7/8/2022.
- Sun Q, Cao H, et al. Biomed Chromatogr. 2016;30(11):1820-1834.
- Hase A, Jung SE, et al. Pharmacol Biochem Behav. 2015;133:1-6.
- Lopresti AL, Smith SJ, et al. Medicine. 2019;98(37):e17186.


