In times of serious health alarm as has been happening in the COVID-19 pandemic, the burden on the healthcare system and families has expanded. The current pandemic is having a profound effect on all aspects of society, including mental and physical health.1 This may be particularly true of family and palliative healthcare workers whose focus is optimizing quality of life and minimizing suffering for seriously or chronically ill individuals.
Living or working in such a stressful environment is an emotionally charged challenge that can affect emotional stability. The quality of care for patients and their relatives may be threatened through long-term absenteeism or a brain and skill drain if the healthcare professionals leave their jobs prematurely in order to preserve their own health.2 To maintain heart-centered sanity and prevent burnout, those caring for the long-term ill must include self-care, self-compassion, and compassion for others as countermeasures.3
What is Compassion?

We know that compassionate care is essential for positive clinical and patient outcomes. The importance of compassion in palliative care is widely recognized and is currently receiving increased research attention. Hoffman et al, define compassion as an emotion that elicits “the heartfelt wish that sentient beings be free from suffering and the causes of suffering.”4 Clara Strauss and colleagues5 propose that compassion consists of five elements:
- recognizing suffering
- understanding the universality of human suffering
- feeling for the person suffering
- tolerating uncomfortable feelings
- motivation to act/acting to alleviate suffering
There has been increasing concern, however, that the expression of compassion as a value in palliative care is being compromised.3 This situation has come to be called Compassion Fatigue. It was first introduced as a description for nursing burnout6 and is characterized as the development of emotional, physical, and/or spiritual exhaustion as a result of working with traumatized individuals.7 Compassion fatigue may even have signs and symptoms that mirror PTSD.8 A variety of stressful factors and negative affect promote compassion fatigue and burnout, whereas positive affect is helpful in achieving compassion satisfaction.9 Researchers have pointed out that oncologists and other palliative care workers who deal with loss on a regular basis may also have unprocessed grief that can lead to compassion fatigue and burnout.8
Burnout, which may or may not be a separate state, involves a progressive loss of idealism, energy, and purpose experienced by people in the helping professions as a result of the conditions of their work. It is further defined by three key characteristics: physical and emotional exhaustion, cynicism, and inefficacy.8 In clinicians working with seriously ill cancer patients, the rates of all three characteristics of burnout are high, with up to
- 69% of oncologists experiencing emotional exhaustion
- 10% – 25% of oncologists experiencing depersonalization which is a form of cynicism
- 33% – 50% of oncologists and palliative care physicians reporting inefficacy
Who is at Risk of Experiencing Compassion Fatigue and Burnout?
As human beings, we are all at risk to some extent. This may be particularly true when family members become chronically ill and require extended care. A family member with diabetes, Alzheimer’s Disease, or even advanced age can require our compassionate care over time. Moreover, all physicians and other palliative care workers can be at risk for compassion fatigue and burnout as a result of both work and personal characteristics.
Work factors include:8
- Work overload (e.g., large patient volumes, insufficient resources, or feeling poorly managed)
- Lack of control over one’s work environment
- Having the bulk of one’s time at work spent on tasks inconsistent with one’s career goals
- High levels of work-home interference
Personal factors may include: 8
- Being female
- Working in a solo practice
- Being early in one’s career
- Lacking a sense of personal control over events
- Attributing success to chance instead of personal accomplishments
- Lack of awareness in recognizing the personal emotional toll of caring for dying patients
Maintaining Compassion
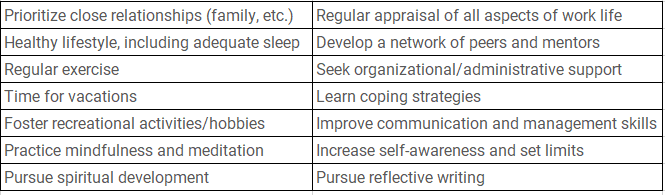
A wide range of intervention strategies has emerged in the research literature. Vachon and colleagues have highlighted a link between self-care and self-compassion and argued that self-compassion is a prerequisite for compassion for others.3 Within the caring professions, self-care is associated with resilience and burnout prevention, whilst a lack of self-care has been linked to compassion fatigue.10 However, such a valuable focus on self-care seems to be missing. In the accreditation standards for US and Canadian medical schools, the Liaison Committee on Medical Education found that no published curriculum focused specifically on self-care.8
Personal Self-Care
Personal self-care starts with the recognition that people have multiple personal dimensions to attend to in order to live a “good” life, including inner lives, families, work, community, and spirituality.8 Professional self-care builds on the foundation of well-crafted personal self-care.
Personal Self-Care Strategies8 Professional Self-Care Strategies7
Compassion Fatigue and Neurotransmitters
Compassion fatigue and associated symptoms are a sign of stress linked to providers who care for the chronically or terminally ill. When combined with a lack of personal and/or professional self-care, this stress can easily imbalance our neurotransmitters and hormones. The resulting imbalances can lead to anxiousness, sadness, irritability, sleep issues and more which can further worsen the ability to express compassion.
Whether you are palliative healthcare provider or a family member providing care to a loved one, become your own patient first – measure your neurotransmitters and hormones, rebalance yourself and implement strategies to live that “good life.”
References
- Franza F, et al. Psychiatria Danubina. 2020; Vol. 32, Suppl. 1, pp 10-14.
- van Mol MMC, et al PLoS One. 2015; 10(8): e0136955.
- Mills, J et al. International Journal of Palliative Nursing. 23(5), pp. 219-229.
- Hofmann SG, et al. Clin Psychol Rev. 2011 Nov; 31(7): 1126–1132.
- Strauss C, et al. Clinical Psychology Review. 2016 July; 47:15-27.
- Cross LA. J Hosp Palliat Nurs. 2019 Feb; 21(1): 21–28.
- Alharbi J, et al. Saudi Med J. 2019 Nov; 40(11): 1087–1097.
- Sanchez-Reilly S, et al. J Support Oncol. 2013 Jun; 11(2): 75–81.
- Zhang Y, et al. Medicine (Baltimore). 2018 Jun; 97(26): e11086.
- Figley CR. Journal of Clinical Psychology. 2002 Nov; 58(11):1433-1441.


